How to Choose the Right Quantitative Neuromuscular Monitor
Step 1: Start With the Clinical Requirement—Not the Technology
With the release of the 2023 Practice Guidelines for Monitoring and Antagonism of Neuromuscular Blockade from the American Society of Anesthesiologists, anesthesia departments are now expected to routinely use quantitative neuromuscular monitoring whenever non-depolarizing neuromuscular blocking agents are administered.
The goal of these guidelines is clear: Confirm adequate recovery (TOF ratio ≥ 0.9) prior to extubation to reduce postoperative respiratory complications.
Importantly, the guidelines were delayed for years—not due to lack of evidence—but due to concerns that older quantitative monitors were too difficult, unreliable, or disruptive to routine workflow. As summarized in the 2018 international consensus statement:
“A major limitation to widespread adoption of objective neuromuscular monitors is not their cost, but their ease of use… New monitors that are reliable, easy to set up, and produce repeatable responses are needed.”1

Figure 1: A mechanomyograph as shown in a 1976 Anesthesiology article5.
The 2023 guidelines acknowledge that this barrier is now changing with the introduction of substantially improved technology.2
Key takeaway:
Before comparing features or prices, ensure the device can reliably support guideline-level decision-making in real clinical conditions.
Step 2: Understand What All Quantitative Monitors Are Trying to Measure
All quantitative neuromuscular monitors share the same physiological goal: Measure the muscle’s response to peripheral nerve stimulation and express recovery as a Train-of-Four (TOF) ratio. As demonstrated by Eikermann, even modest levels of residual neuromuscular blockade (TOF ratios as high as 80%) may cause significant airway narrowing3.

Figure 2: Minimum retroglossal upper airway diameter during forced inspiration (A) before neuromuscular blockade (baseline), at a steady-state TOF ratio of (B) 0.5 and (C) 0.8. Images from the volunteer show that a partial paralysis evokes an impairment of upper airway diameter increase during forced inspiration. *p < 0.05 versus baseline.3
What differs is how that response is detected.
Historically and currently, the following technologies have been used:
- Mechanomyography (MMG) – Measures force of contraction
- Electromyography (EMG) – Measures muscle electrical activity
- Acceleromyography (AMG) – Measures acceleration of thumb movement
Why this matters:
MMG is the reference gold standard used to define TOF ≥ 0.9 as adequate recovery. Any monitor used clinically should produce results that are equivalent to MMG4.
Step 3: Recognize Why First-Generation Quantitative Monitors Struggled
Mechanomyography: Accurate but Impractical
MMG established the science of neuromuscular recovery but required rigid arm fixation, preload weights, and specialized setup—making it unsuitable for routine OR use.
Acceleromyography: Practical but Fundamentally Limited
To overcome MMG’s impracticality, many first-generation clinical monitors adopted acceleromyography (AMG). While easier to deploy, AMG introduced two major problems5:
- Requires unrestricted thumb movement
– Difficult or impossible with tucked arms, surgical draping, or positioning constraints. - TOF ratios are not equivalent to MMG
– Baseline TOF ratios often exceed 1.0
– Recovery must be manually “normalized” using a pre-block baseline
As summarized in the referenced literature:
- Without a baseline measurement, true recovery cannot be reliably determined.
- Normalization is inconsistently performed in real-world practice.
- AMG may overestimate recovery, increasing the risk of residual blockade.
Key takeaway:
A monitor that requires manual correction or ideal limb positioning undermines the very safety goal it is meant to support.
Step 4: Evaluate Modern EMG—But Know That Not All EMG Is the Same
Advances in electronics and signal processing have enabled second-generation EMG-based monitors, which overcome many historical limitations of AMG.
Advantages of modern Electromyography:
- Does not require unrestricted thumb movement
- Produces TOF ratios equivalent to mechanomyography
- Allows monitoring during deep blockade through recovery
- Works with tucked arms and varied positioning
- Noise misinterpreted as muscle activity (phantom twitches)6
- Over-filtering that suppresses true twitches (undercounting)7
However, EMG introduces a new challenge: electrical noise.
The EMG signal is small and exists in an electrically noisy OR environment. Poor signal handling can lead to:
Experts have therefore emphasized:
“The performance of commercially available twitch monitors should be compared to mechanomyography, using mechanomyography as the reference gold standard.”5
%20monitoring%20devices..png?width=3046&height=1922&name=Simultaneous%20measurements%20from%20two%20electromyography%20(EMG)%20monitoring%20devices..png)
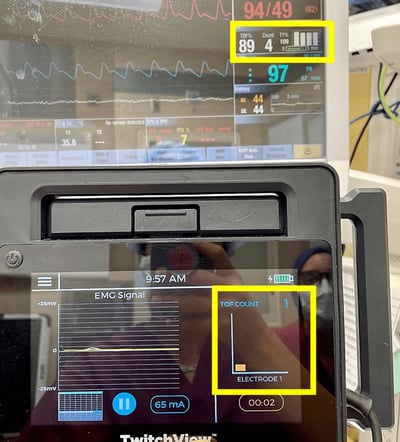
Figure 3: Simultaneous measurements from two electromyography (EMG) monitoring devices. TwitchView portrays expected linear recovery while EMG Monitor 2 underestimates recovery. EMG monitor 2 fails to measure post-tetanic count (PTC) and undercounts twitches.7
Key takeaway:
Choosing “EMG” is not enough. The system must be clinically validated against MMG across all depths of blockade.
Step 5: Demand Clinical Validation—Not Just Technical Claims
Not all EMG monitors are validated under conditions that reflect routine clinical practice. Some devices demonstrate performance in controlled laboratory or research environments, where patient positioning is ideal, electrical interference is minimal, and monitoring is managed by trained investigators rather than busy clinical teams.
While such testing may establish technical feasibility, it does not necessarily predict reliability in the operating room, where electrocautery, warming devices, patient movement, variable electrode placement, and time pressure are routine.
Clinically meaningful validation requires demonstration that a monitor provides stable, interpretable data across a range of patients and surgical conditions, when used by typical anesthesia providers, and incorporated into standard workflows. Without evidence of performance in real-world OR settings, technical specifications alone are insufficient to support adoption as a routine clinical tool.
What counts as clinical validation?
When evaluating a quantitative neuromuscular monitor, look for evidence that it has been:
- Studied in routine operating room environments, not only research settings
- Evaluated by independent, third-party investigators
- Shown to provide stable TOF ratio values during electrocautery, warming, and patient movement
- Demonstrated outcomes to be reproducible across different users and cases
- Assessed at clinically relevant decision points, particularly during emergence and extubation
- Integrated into standard anesthesia workflows, not just controlled research protocols
If these criteria are not met, technical specifications alone are unlikely to predict real-world reliability.
Step 6: Assess Workflow Fit and Ease of Adoption
Finally, technology only improves outcomes if it is used consistently.
Despite access to quantitative monitors, many clinicians skip using them, relying on sugammadex as a safety net instead.
However, a large database study showed that while sugammadex reduced residual neuromuscular blockade compared with neostigmine—complete elimination of respiratory complications required quantitative neuromuscular monitoring.8
Independent studies of universal quantitative monitoring show why this matters. In one academic medical center analysis, 60% of patients judged ready for extubation using qualitative assessment still had a TOF ratio < 0.9—placing them at risk for postoperative pulmonary complications.9
Even modest reductions in postoperative pulmonary complications were projected to more than offset the cost of universal quantitative monitoring, making accuracy not only a clinical issue—but an operational one.
When evaluating monitors, ask:
- Does setup take seconds—or minutes?
- Does performance depend on positioning?
- Does it require the clinician to click through multiple screens for key information?
- Can it be used reliably across patient sizes?
- Will clinicians trust and adopt it?
Ease of use was explicitly cited as the primary barrier to adoption—not cost.
Putting It All Together: A Practical Decision Framework
When choosing a quantitative neuromuscular monitor, prioritize:
- Guideline alignment: Supports TOF ≥ 0.9 confirmation using approved muscle sites (adductor pollicis, first dorsal interosseus, and flexor hallucis brevis).
- Measurement method: Prefer electromyography (EMG) over Acceleromyography (AMG).
- Gold-standard validation: Interchangeable with MMG.
- Noise cancelling: Separates true signal from OR noise, accurate through all levels of blockade.
- Workflow reliability: Works in real OR conditions, in any setup environment. Not just perfect research conditions.
- Adoption potential: Easy enough to become routine.
Final Thought:
The 2023 ASA guidelines marked a turning point. Quantitative neuromuscular monitoring is recommended as the standard of care—but not all monitors are equally capable of delivering the safety the guidelines demand.
Choosing the right technology isn’t just about buying a monitor—it’s about selecting one that provides all the data that is needed and can be easily accessed and used.
When evaluating a new monitor, ask yourself “Can I trust what the monitor is telling me at the moment it matters most?”
Learn why the TwitchView® Train of Four Monitor sets the gold standard for EMG based monitors.8 9
TwitchView® has been clinically validated in several independent, third-party hospital settings, where performance is assessed under routine clinical conditions. These validations extended beyond technical noise cancellation for accurate EMG signal detection to clinically relevant measures, including customized management of neuromuscular blockade through trended data, guidance of reversal agent selection, and analysis of postoperative pulmonary outcomes and cost of care.9 10 11
- Naguib M, et al. Consensus statement on perioperative use of neuromuscular monitoring. Anesth Analg. 2018;127(1):71-80.
- Thilen SR, et al. 2023 American Society of Anesthesiologists practice guidelines for monitoring and antagonism of neuromuscular blockade. Anesthesiology. 2023;138:13-41.
- Eikermann M, et al. Predisposition to inspiratory upper airway collapse during partial neuromuscular blockade. Am J Respir Crit Care Med. 2007;175(1):9-15.
- Claudius C, et al. Acceleromyography for use in scientific and clinical practice: a systematic review of the evidence. Anesthesiology. 2008;108:1117-1140.
- Bowdle A, et al. Progress toward a standard of quantitative twitch monitoring. Anaesthesia. 2020;75(9):1133-1135.
- Bowdle A, et al. Quantitative twitch monitoring: what works best and how do we know? Anesthesiology. 2021;135:558-561.
- Bussey L, et al. Train-of-four monitoring with the TwitchView electromyograph compared to the GE NMT electromyograph and manual palpation. J Clin Monit Comput. 2020.
- Bussey L, et al. Pilot study of train-of-four and post-tetanic count monitoring with the TetraGraph electromyograph compared to the TwitchView monitor. medRxiv. 2021.
- Wachtendorf LJ, et al. Changes in intraoperative rocuronium dosing following introduction of sugammadex and association with postoperative respiratory complications. Anesthesiology. 2025.
- Edwards LA, et al. Universal quantitative neuromuscular blockade monitoring at an academic medical center: impact on clinical outcomes and cost of care. Perioper Care Oper Room Manag. 2021.
- Bowdle TA, et al. Dose-finding study of sugammadex for reversal of rocuronium in cardiac surgery patients and postoperative monitoring for recurrent paralysis. Anesthesiology. 2023;139(1):6-15.
- Thilen SR, et al. Management of muscle relaxation with rocuronium and reversal with neostigmine or sugammadex guided by quantitative neuromuscular monitoring. Anesth Analg. 2023;139(3):536-544.