Where You Measure Matters: The Truth About TOF Monitoring Sites

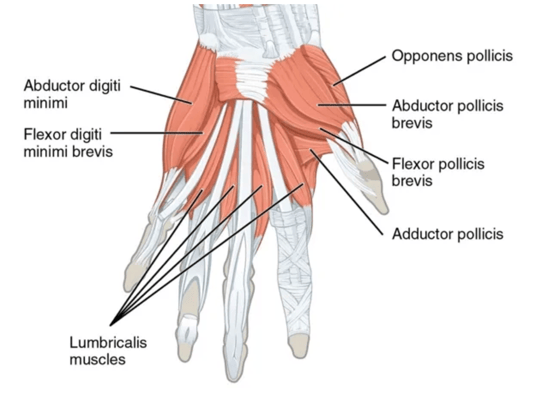
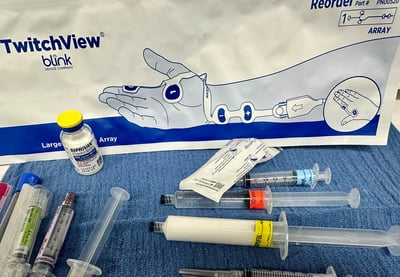
Figure 1. The adductor pollicis and abductor digiti minimi shown on this view of the palm of the hand. The first dorsal interosseous is shown in Figure 2.
Three muscles in the hand innervated by the ulnar nerve have been used to quantitatively monitor the response to train-of-four stimulation with electromyography. These are the adductor pollicis, the first dorsal interosseous and the abductor digiti minimi. The adductor pollicis is on the palmar side of the thumb while the first dorsal interosseous is on the back side of the thumb as shown in the illustrations. The abductor digiti minimi lies along the little finger as shown.
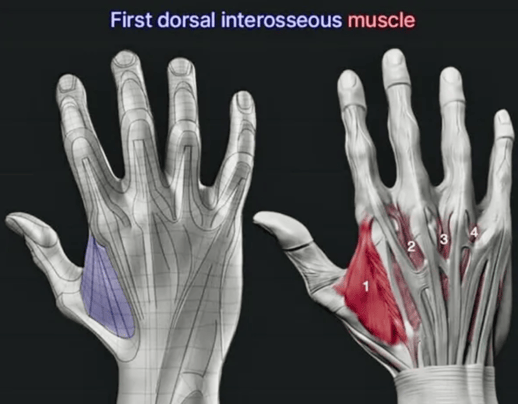
Figure 2. First dorsal interosseous is located on the back of the hand essentially opposite the adductor pollicis.
Does it matter which one of these muscles we use for monitoring? Traditionally, the adductor pollicis has been used most frequently. Let’s first look at the recently published American Society of Anesthesiologists practice guidelines on monitoring neuromuscular blockade. The guidelines document has the following statement—
The reference site of measurement is the adductor pollicis muscle. Train-of-four ratios at the adductor pollicis and first dorsal interosseous muscles are similar when measured simultaneously, and therefore, it appears reasonable to use data interchangeably between these sites, especially if the adductor pollicis muscle is not available or signal quality is poor. Train-of-four ratios at the adductor pollicis muscle are lower than the abductor digiti minimi when measured simultaneously, indicating a relative resistance to neuromuscular blockade at the abductor digiti minimi. Therefore, data from the abductor digiti minimi muscle should be used with caution to guide neuromuscular blockade management (understanding the patient is more deeply paralyzed than the monitor indicates).
Interestingly, this statement is not referenced. It turns out that there are not a lot of data on this subject, but there are some. Let’s look at what the data shows.
The first digital interosseus muscles performs quite well in several studies
Harper published a study in the British Journal of Anaesthesia in 1988 comparing the electromyogram of the adductor pollicis to the first dorsal interosseous during neuromuscular blockade with atracurium or vecuronium. He found no significant differences between the adductor pollicis and the first dorsal interosseous in time to onset of block, time to recovery or train-of-four ratio at maximum block.
Kalli also published in the British Journal of Anaesthesia in 1990, comparing the electromyograms of the adductor pollicis, first dorsal interosseous and abductor digiti minimi, in the absence of neuromuscular blockade. He found that the first dorsal interosseous had the electromyogram with the largest amplitude, 1.5 times larger than either the adductor pollicis or the abductor digiti minimi. On that basis, he recommended the first dorsal interosseous for routine monitoring.
Philips et al studied all 3 muscles during recovery from block with rocuronium using the GE electromyograph. While this device isn’t our preferred system—we previously published a study showing that the GE had difficulty distinguishing noise from EMG signals - back in 2012, when Philips et al conducted their study, it was really the only game in town. Since then, better alternatives for electromyography have become available. Philips found that the adductor pollicis and first dorsal interosseous were very similar, with no bias in Bland-Altman analysis. The abductor digiti minimi was more resistant to neuromuscular blockade, so that when the train-of-four ratio at the adductor pollicis and first dorsal interosseous was 0.8, the train-of-four ratio at the abductor digiti minimi was 0.9.
The performance of the abductor digiti minimi seems less certain
Iwasaki et al compared the abductor digiti minimi response measured with electromyography to the adductor pollicis response measured with acceleromyography. This study design is problematic, as numerous prior investigations have shown that acceleromyography and electromyography will likely get quite different results because of the “overshoot” in the acceleromyograph train-of-four ratio and the relative lack of precision of acceleromyography. So this is a bit of a comparison of apples and oranges. It’s pretty much impossible to know whether any differences in the two monitoring sites are due to differences in the muscle response or differences in the monitors used or both. They found that recovery to a post tetanic count of 1, a train-of-four count of 1 and a train-of-four count of 2 occurred more quickly when judged by acceleromyography of the adductor pollicis, compared to recovery judged by electromyography of the abductor digiti minimi. The time to a train-of-four ratio (normalized for the acceleromyography) of at least 0.9 was not different. In my opinion, the confounding effect of using different types of monitoring for the 2 muscles makes these results difficult to interpret.
Iwasaki et al conducted another similar study but using electromyography to assess both the adductor pollicis and the abductor digiti minimi (Figure 3). This study, like the Philips et al. study is a much better design than the first Iwasaki study described above in which different monitoring modalities were used for the 2 muscles. In this study, they measured the time to recovery of a post tetanic count of 1, a train-of-four count 1 or 2 and a train-of-four ratio of 0.9. They reported mixed results, with the abductor digiti minimi recovering a post tetanic count of 1 faster than the adductor pollicis, but the time to reach a train-of-four ratio of 0.9 was similar between the two muscles.
 Figure 3. An electromyogram electrode array with the sensing electrode on (A) the adductor pollicis and (B) the abductor digiti minimi from Iwasaki et al.
Figure 3. An electromyogram electrode array with the sensing electrode on (A) the adductor pollicis and (B) the abductor digiti minimi from Iwasaki et al.
Another study comparing the adductor pollicis and abductor digiti minimi has been performed by Nagy et al and has been presented as an abstract (ESIAC 2025 meeting) but has yet to be published as a peer reviewed manuscript.
What should we conclude about the abductor digiti minimi from these published studies and an abstract? The available data are relatively sparse, and the results are a bit murky.
What muscles do current quantitative monitors use?
It is relevant to look at how the commonly available electromyography electrode arrays interact with these 3 muscles. The standard (“large”) TwitchView electrode array has a sensing electrode over both the adductor pollicis and the first dorsal interosseous--the two muscles recommended in the ASA guidelines and found by Philips et al to be essentially interchangeable (Figure 4). The TwitchView TOF Monitor will automatically select the sensing electrode with the highest amplitude signal, or the user can manually select one or the other*. All of the other available electrode arrays, including the TwitchView “medium” and “small” electrode arrays, can be placed over the adductor pollicis or the abductor digiti minimi.
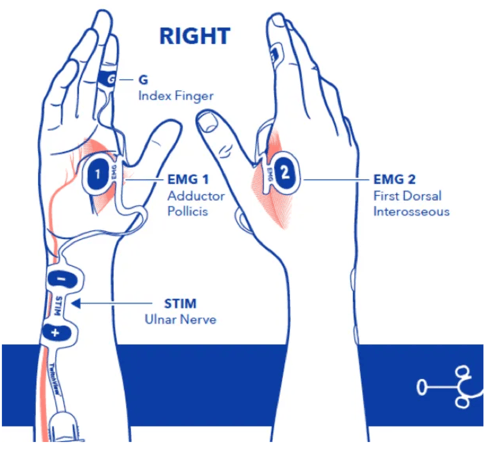
Figure 4. The standard (“large”) TwitchView electrode array is capable of sensing either the adductor pollicis (1) or the first dorsal interosseous (2)
Which muscles should we use?
Are the adductor pollicis, first dorsal interosseous and abductor digiti minimi equivalent for neuromuscular block monitoring? Maybe they are and maybe there are some differences. If there are differences, are they clinically significant? We don’t really know for sure. For now, I recommend monitoring the adductor pollicis or the first dorsal interosseous, the two muscles recommended by the ASA guidelines.
One thing that has been answered definitively is that stimulating the facial nerve and monitoring muscles around the eye is not reliable and can easily lead to thinking a patient is recovered from neuromuscular blockade when in fact they are not. The American Society of Anesthesiology practice guidelines recommends against monitoring eye muscles.
*If the user manually sets the stimulating current (rather than having the machine automatically determine the suprmaximal current), electrode 1 will be the sensing electrode. However, the user can still manually select electrode 2 if desired.

Adapted with permission from Andrew Bowdle MD, PhD, FASE. Originally published on Dr. Bowdle's Substack
A Higher Plane of Anesthesia.
- Kaufhold N, Schaller SJ, Stäuble CG, Baumüller E, Ulm K, Blobner M, Fink H. Sugammadex and neostigmine dose-finding study for reversal of residual neuromuscular block at a train-of-four ratio of 0.2 (SUNDRO20)†, Br J Anaesth. 2016 Feb;116(2):233-40.
- Fuchs-Buder T, Meistelman C, Alla F, Grandjean A, Wuthrich Y, Donati F. Antagonism of low degrees of atracurium-induced neuromuscular blockade: dose-effect relationship for neostigmine. Anesthesiology. 2010 Jan;112(1):34-40.
- Kim KS, Cheong MA, Lee HJ, Lee JM. Tactile assessment for the reversibility of rocuronium-induced neuromuscular blockade during propofol or sevoflurane anesthesia. Anesth Analg. 2004 Oct;99(4):1080-1085.
- Ebert TJ, Cumming CE, Roberts CJ, Anglin MF, Gandhi S, Anderson CJ, Stekiel TA, Gliniecki R, Dugan SM, Abdelrahim MT, Klinewski VB, Sherman K. Characterizing the Heart Rate Effects From Administration of Sugammadex to Reverse Neuromuscular Blockade: An Observational Study in Patients. Anesth Analg. 2022 Oct 1;135(4):807-814.
- Herbstreit F, Zigrahn D, Ochterbeck C, Peters J, Eikermann M. Neostigmine/glycopyrrolate administered after recovery from neuromuscular block increases upper airway collapsibility by decreasing genioglossus muscle activity in response to negative pharyngeal pressure. Anesthesiology. 2010 Dec;113(6):1280-8.
- Payne JP, Hughes R, Al Azawi S. Neuromuscular blockade by neostigmine in anaesthetized man. Br J Anaesth. 1980 Jan;52(1):69-76.