How to Implement the ASA Practice Guidelines for Neuromuscular Blockade

Access Our NMB Reversal Guide PDF - Supports Reversal Drug and Dosage Decisions
The ASA House of Delegates approved practice guidelines for neuromuscular blockade in October 2022. The ASA practice guidelines, a report written by the American Society of Anesthesiologists Task Force on Neuromuscular Blockade was published in the January 2023 issue of Anesthesiology. The publication adds the ASA to a growing consensus of societies recommending quantitative over qualitative neuromuscular monitoring [1].
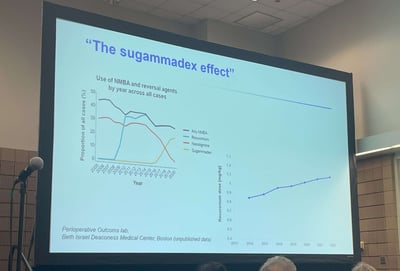
Contrary to the common misconception that sugammadex has eliminated the clinical need for quantitative train of four monitors, utilization of quantitative neuromuscular monitoring is critical to implement the evidence-based recommendations outlined in the guidelines.
As stated by the ASA practice guidelines first author, Dr. Stephan Thilen,
Prior to sugammadex, the rate of residual neuromuscular blockade was 40-60%, which means that our pre-sugammadex practices worked for 40-60% of patients. As such, there is still a place for neostigmine and spontaneous recovery in today’s practice of anesthesia.
Neuromuscular Blockade Reversal Guides
The ASA neuromuscular monitoring guidelines define clinically relevant levels of neuromuscular blockade and include recommended antagonism for each level, providing concrete guidance for the creation of reversal protocols or decision support guides, such as rocuronium reversal guide below, which is supplied to all TwitchView train of four monitor users to aid monitor utility.
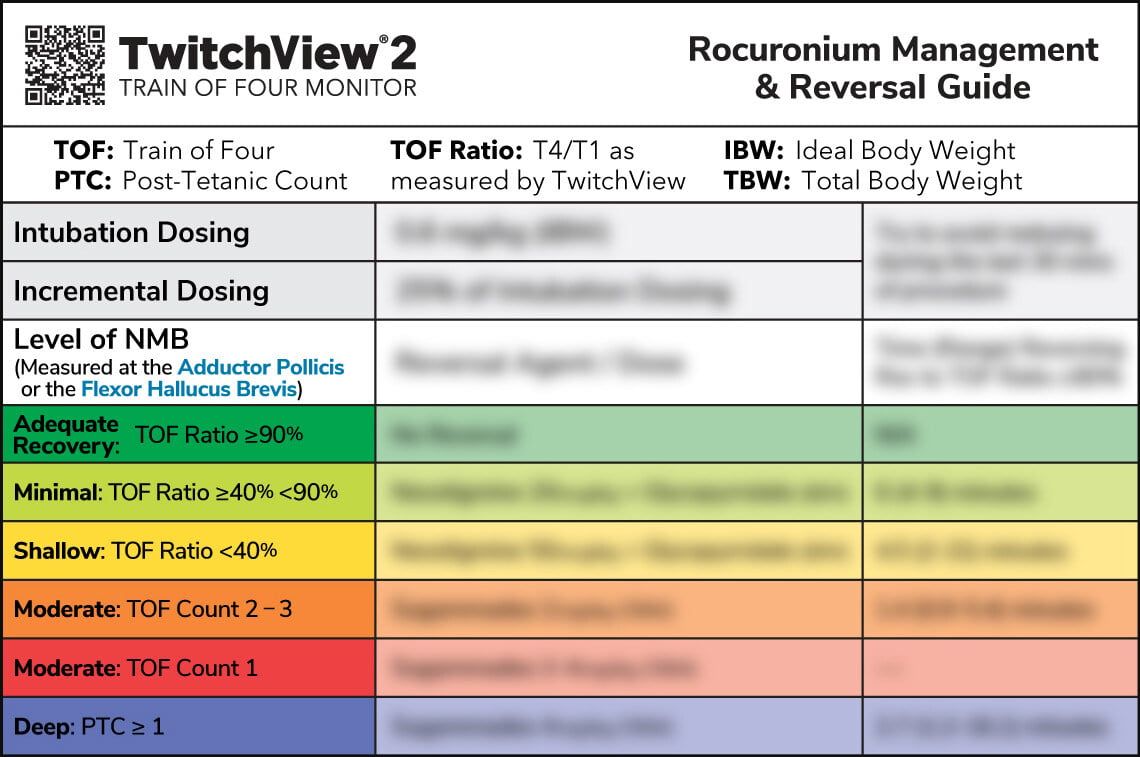
Of note, the recommendations include the appropriate use of neostigmine and abstention of pharmacological reversal if the patient has spontaneously recovered to a TOF ratio ≥90% —made possible by quantitative neuromuscular monitoring.
While quantitative monitoring provides more accurate data than subjective assessments, the onus to implement this data into clinical practice and realize the patient safety benefits remains with the clinician. To avoid residual neuromuscular blockade, the following practice is key:
Confirm a TOF ratio greater than or equal to 0.9 at the adductor pollicis before extubation.
Decrease Sugammedex Dosing
Beyond confirmation of adequate recovery, early adopters of quantitative neuromuscular monitoring like Dr. Thilen have found that they are able to alter neuromuscular blockade management using the continuous data provided by quantitative monitors [2, 3].
Speaking of his own study, Dr. Thilen noted, Using an EMG-based quantitative neuromuscular monitor and a decision support guide, we achieved a 0% incidence rate of residual neuromuscular blockade, while using sugammadex for less than 50% of all patients. Approximately 20% of the patients in our mixed surgical population achieved adequate spontaneous recovery and did not need any pharmacological reversal [3].
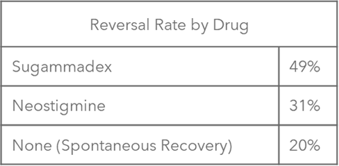
Figure 1: The overall utilization rate for reversal modalities in Dr. Thilen's research.
Practice adjustments include administration of smaller neuromuscular blocking agent intubation doses and smaller more frequent intraoperative redoses of 2-5 mg of rocuronium to maintain tighter control, while still preserving optimal surgical conditions. Such reductions in cumulative NMBA use are thought to enable the safe utilization of neostigmine or abstention from pharmacological reversal when the patient spontaneously recovers to a TOF ratio ≥90%, as recommended by the ASA guidelines.
An example of such neuromuscular blockade management is pictured in the TwitchView TOF monitor trend plot below. A 63 y/o patient was undergoing fusion of the anterior cervical vertebra C4-5 with ACDF under microscope. The surgeon requested minimal neuromuscular blockade citing their goal to minimize the patient’s response to surgical stimuli whilst mitigating potential trauma of the recurrent laryngeal and cervical nerves during the anterior dissection.
Using the continuous data from TwitchView and feedback from the surgeon, the anesthesia provider determined a TOF count 3 provided ideal conditions and titrated blockade accordingly. The patient was reversed with neostigmine and a TOF Ratio of 100% was achieved prior to extubation. Blink Device Company, creators of the TwitchView quantitative neuromuscular monitor have developed a suite of educational tools to support customers as they incorporate the monitors into routine care.
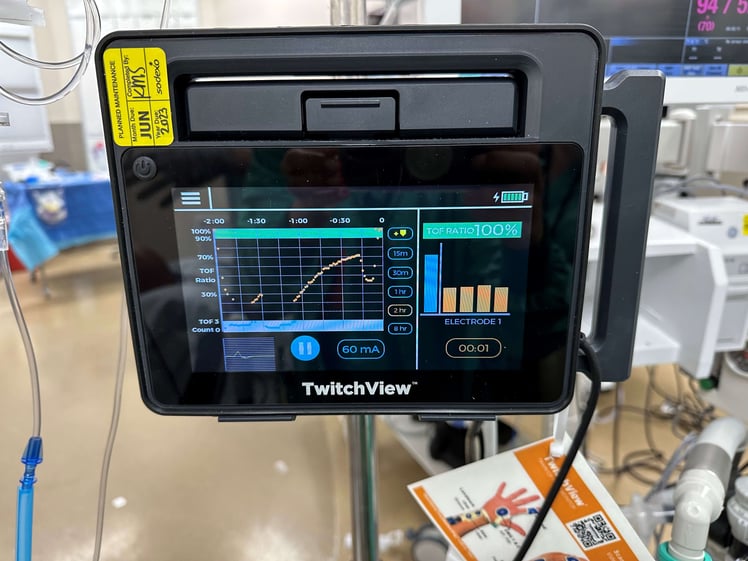 Figure 2: Pictured two-hour trend plot window displaying induction plus 3 maintenance doses of rocuronium and reversal on left and TOF Ratio 100% on right of the TwitchView screen.
Figure 2: Pictured two-hour trend plot window displaying induction plus 3 maintenance doses of rocuronium and reversal on left and TOF Ratio 100% on right of the TwitchView screen.
Understanding that new technology adoption and changes in practice will require time and training, multiple educational opportunities across several different platforms are expected to release in the 2023 calendar year. The following list contains current recommended educational content, and we will share new opportunities as they emerge.
Neuromuscular Blockade Educational Resources
Literature:
- 2023 ASA Practice Guidelines for Monitoring and Antagonism of Neuromuscular Blockade
- Consensus Statement on Perioperative Use of Neuromuscular Monitoring
- Conceptual and technical insights into the basis of neuromuscular monitoring
Active CME Activities:
- ASA Monitoring Neuromuscular Blockade 2023
- Reverse to Go Forward? Safe Neuromuscular Blockade and Reversal in the Perioperative Setting
- Stanford Anesthesia: Neuromuscular Monitoring
Podcasts:
- APSF Episode #84 Episode Keeping Patients Safe and Strong with Quantitative Neuromuscular Monitoring
- Depth of Anesthesia: How do you reverse neuromuscular blockade? – Part 1 of 2
- Stephan R. Thilen, Wade A. Weigel, Michael M. Todd, Richard P. Dutton, Cynthia A. Lien, Stuart A. Grant, Joseph W. Szokol, Lars I. Eriksson, Myron Yaster, Mark D. Grant, Madhulika Agarkar, Anne M. Marbella, Jaime F. Blanck, Karen B. Domino; 2023 American Society of Anesthesiologists Practice Guidelines for Monitoring and Antagonism of Neuromuscular Blockade: A Report by the American Society of Anesthesiologists Task Force on Neuromuscular Blockade. Anesthesiology2023; 138:13–41 doi: https://doi.org/10.1097/ALN.0000000000004379
- Edwards LM, Ly NK, Shinefeld J, Morewood GH. (2021), Universal quantitative neuromuscular blockade monitoring at an academic medical center—A multimodal analysis of the potential impact on clinical outcomes and total cost of care. Perioperative Care and Operating Room Management, Volume 24,100184, ISSN 2405-6030, https://doi.org/10.1016/j.pcorm.2021.100184.
- Thilen SR, Sherpa J, Treggiari MM, James A, Cain KC, Bhananker SM. Best Management of Muscle Relaxation with Rocuronium Using Objective Monitoring and Reversal with Neostigmine or Sugammadex. Oral presentation Feb 28, 2020, Whistler Anesthesia Summit, Whistler, BC, Canada