Anesthesia Experts Recommend These 4 Steps to Implement Quantitative Train of Four Monitoring
With the adoption of the 2023 ASA Practices Guidelines for Monitoring and Antagonism of Neuromuscular Blockade on the rise, members of the ASA and ESAIC task forces published four recommendations for anesthesia departments looking to implement quantitative neuromuscular monitoring[1].
The exact strategies employed by any given practice may vary, but a systematic approach may include:- A quantitative monitor in every anesthetizing location.
- Educational efforts on the departmental and individual levels utilizing different mediums.
- Performance feedback on the departmental and individual levels.
- The presence of a local champion who is supported by the departmental and institutional leaders.
Given our sole focus on quantitative neuromuscular monitoring and our experience supporting hospital implementations worldwide, we emphatically agree with these recommendations. Working with our hospital partners, we have learned that the key to successful implementation is to create a plan customized to each hospital’s unique culture, which includes four pillars of implementation:
 Figure 1: Four Pillars of an Effective Implementation
Figure 1: Four Pillars of an Effective Implementation
Let's explore the pillars in further detail.
1. Access to Quantitative Neuromuscular Technology
Having a monitor in most, if not all, anesthetizing locations sets the standard of care for your institution. For decades, the market lacked reliable, easy-to-use quantitative technologies. With second-generation EMG devices, like TwitchView, the new hurdle is budget allocation. Equipping every OR with a monitor may have a high initial cost. At Blink, we help customers analyze their institution's potential savings on NMBA, reversal agents, and the cost of post-operative complications to justify and offset the capital and consumable expenses.
A study by Edwards et al. determined that the cost of implementing quantitative monitors was far less than the cost of post-operative complications, enabling the health system to standardize TwitchView in every OR across the hospital system.
The maximum potential cost savings for Temple University Hospital derived from eliminating post-operative pulmonary complications associated with residual neuromuscular blockade would be roughly 7 million dollars annually. This compares very favorably with an annual cost of implementing universal [TwitchView] quantitative train of four monitoring of $162,000 illustrated in Figure 2 [3].
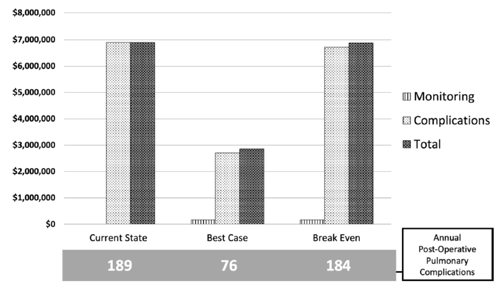 Figure 2: Temple University Hospital annual institutional cost of post-operative pulmonary complications without monitoring (current state) vs. the projected reduction in costs with monitoring (best case) or break-even conditions after implementing TwitchView.
Figure 2: Temple University Hospital annual institutional cost of post-operative pulmonary complications without monitoring (current state) vs. the projected reduction in costs with monitoring (best case) or break-even conditions after implementing TwitchView.
2. (Refresh) Education on Principles of Neuromuscular Monitoring and Pharmacology
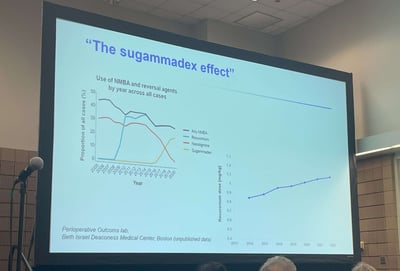
In 2019, a group of neuromuscular blockade subject matter experts conducted an Internet-based multilingual survey to test anesthesiologist's knowledge and ability to manage neuromuscular blocking drugs. See Figure 3 for actual survey contents. 1,629 anesthesiologists from 80 countries completed the 9-question survey.
The respondents correctly answered only 57% of the questions. In contrast, the mean confidence exhibited by the respondents was 84%, which was significantly greater than their accuracy. Of the 1629 respondents, 1496 (92%) were overconfident.
The authors concluded that this overconfidence makes clinicians less likely to modify their clinical practice or seek further guidance on practices related to neuromuscular blockade underscoring the importance of education to drive adoption [6].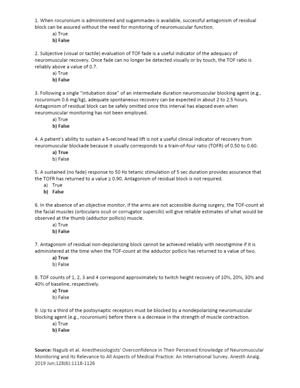 Figure 3: Survey questions/contents.
Figure 3: Survey questions/contents.
Source: 6
Preparing and educating your team is a vital to the implementation process. Collaborate with your device company's clinical expert to develop an education plan that aligns with your department’s culture. Educate your providers on proper device use and reinforce evidence-based clinical information relevant to device application. Set expectations upfront so your team is prepared for what they will encounter in the OR. Continuous quantitative neuromuscular data is a new concept for most providers.
For example, in our experience, providers are often surprised by the occurrence of spontaneous breathing when the monitor is indicating deep levels of blockade. Emphasize that the diaphragm recovers much faster than the hand. A measurement of the adductor pollicis aligns with the pharyngeal muscles which will enable the patient to protect their airway once extubated, not the diaphragm. The monitor is not broken if your patient breathes at a post-tetanic count of 8.
When educating, consider a multifaceted approach to appeal to various learning styles and to reemphasize critical topics (like the diaphragm's ability to function during deep blockade). For example, as noted in a task force report presented at the American Society of Anesthesiologists 2023 annual meeting, NYU Langone Health partnered with Blink to implement a multi-step plan to launch TwitchView system-wide. They started with a Grand Rounds presentation from a quantitative neuromuscular monitoring expert, Dr. Gordon Morewood, Chair at Temple University Hospital. Concurrently, their TwitchView representative provided hands-on intraoperative training and in-services. Assistant Professor Dr. Shah Ahmed at NYU Langone was tasked with continuing education and created an email series to build upon the team’s knowledge and set expectations for standardized monitor use. He included new studies, images, and videos for auditory and visual learners. According to the task force report, by implementing this multi-step plan, NYU Langone's TwitchView utilization contributed to TOF data documentation in over 90% of all cases
 Figure 4: NYU Langone's Department of Anesthesiology, Perioperative Care, and Pain Medicine Grand Rounds Announcement for Dr. Gordon Morewood.
Figure 4: NYU Langone's Department of Anesthesiology, Perioperative Care, and Pain Medicine Grand Rounds Announcement for Dr. Gordon Morewood.
Source: NYU Langone Department of Anesthesiology, Perioperative Care, and Pain Medicine
3. Communication & Feedback on Train of Four Monitor Use
To succeed, the entire interdisciplinary team must be aware of the monitor, why it is being implemented, and its potential positive impact on patient safety and outcomes. Communicate with your team early in the acquisition process. Prepare them for a new parameter, a new standard of care, and emphasize how it will benefit and improve their clinical practice.
Once installed, there will be a ramp-up period. You will have enthusiastic early adopters and their opposite. Consistent feedback improves individual performance— provide feedback department-wide and via personal communications. Include wins, patient case studies, and opportunities for improvement.
Pictured below the Executive Vice Chair of a leading academic institution shares an encouraging update with staff. After combined educational efforts by Blink Device Company and promotional efforts by clinical leadership, anesthesia providers reduced overall utilization of sugammadex by 25%, which translates to a $75,000.00 savings per quarter or $300,000 per year. Of note, a TwitchView train of four monitor is installed in every anesthetizing location across the health system. The achieved results required several months of dedicated effort and show one potential positive outcome when quantitative monitors are routinely used.
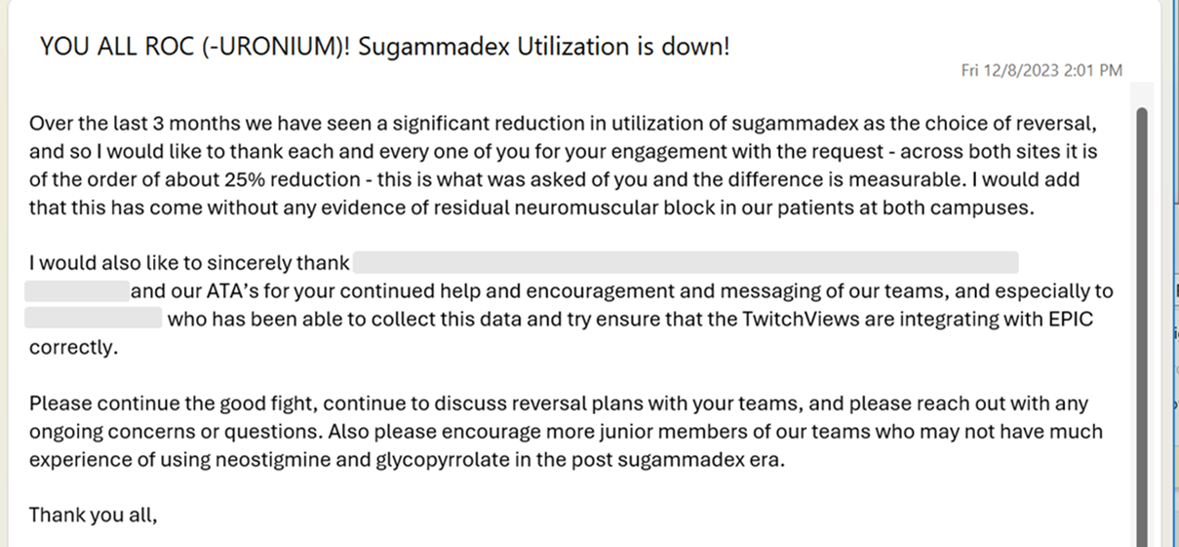 Figure 5: Email announcement from the Executive Vice Chair at a leading academic institution informing staff of the projected $300,000.00 annual savings attributed to education and routine application of the TwitchView train of four monitor.
Figure 5: Email announcement from the Executive Vice Chair at a leading academic institution informing staff of the projected $300,000.00 annual savings attributed to education and routine application of the TwitchView train of four monitor.
Several institutions have employed the Multi-institutional Perioperative Outcomes Group (MPOG) Anesthesiology Performance Improvement and Reporting Exchange (ASPIRE) to improve compliance with their quantitative TOF monitoring. In a study out of Vanderbilt University incorporating Plan-Do-Study-Act (PDSA) and MPOG ASPIRE, compliance with TOF monitoring increased from 42% to 70%.4
4. Train of Four Clinical Champions & Leadership Backing
Designate champions before going live. Enlist team members who are passionate about the subject and who embrace new technology. Task them with coaching, troubleshooting, and offering constructive feedback to their peers. In time, internal champions will emerge. The most powerful advocates are often individuals who resisted adoption initially. It is also incredibly powerful when senior leadership actively participates in the implementation process and serves as clinical champions. An example of this exact scenario follows.
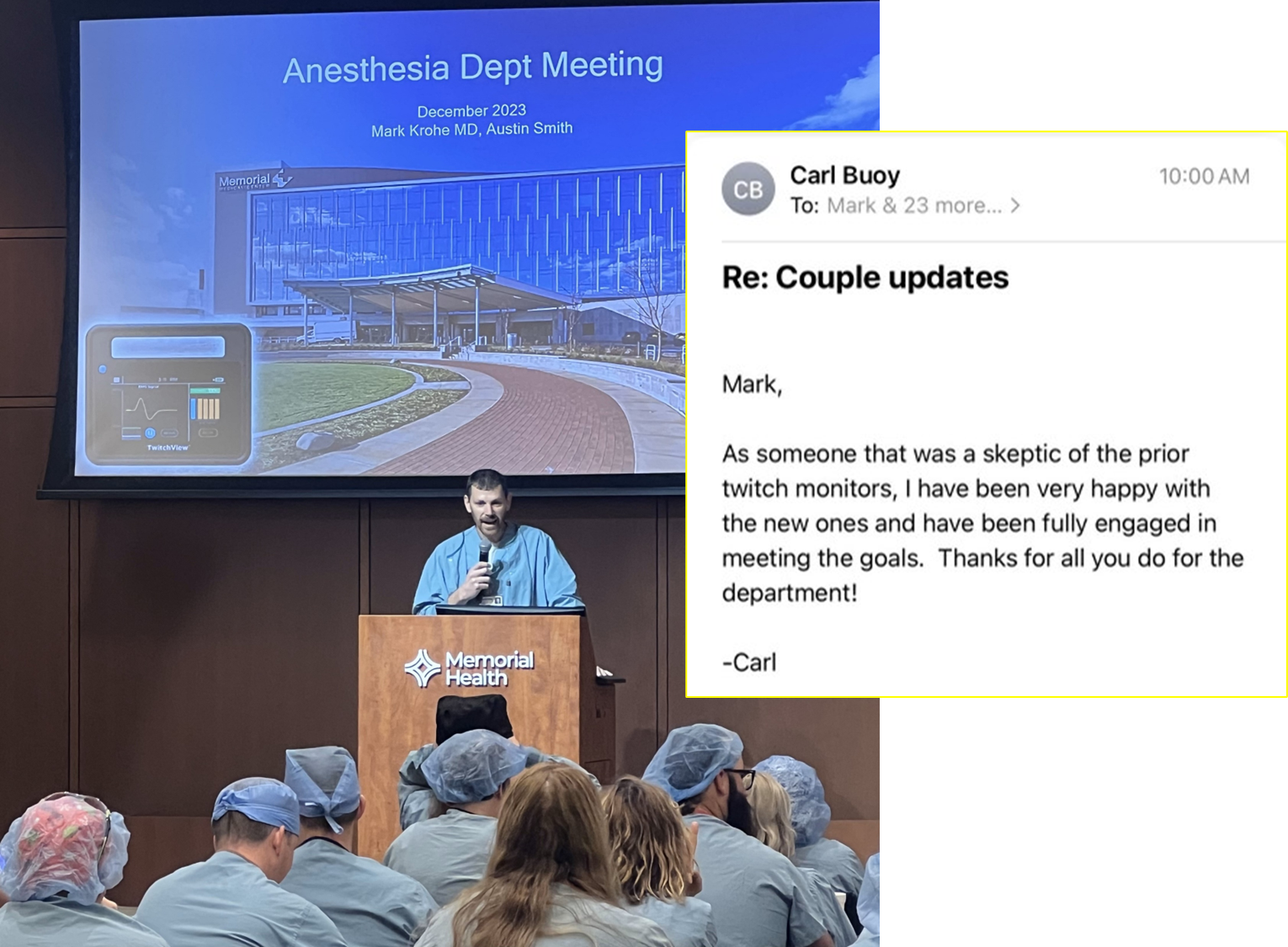 Figure 6: Left: Dr. Mark Krohe with Associated Anesthesiologists of Springfield introduces Memorial Health staff to TwitchView and the system-wide effort to standardize on monitor use. Source: Author; Right: Email communication from the president of the Associated Anesthesiologist of Springfield, Dr. Carl Buoy supporting monitor use and thanking Dr. Krohe for his leadership.
Figure 6: Left: Dr. Mark Krohe with Associated Anesthesiologists of Springfield introduces Memorial Health staff to TwitchView and the system-wide effort to standardize on monitor use. Source: Author; Right: Email communication from the president of the Associated Anesthesiologist of Springfield, Dr. Carl Buoy supporting monitor use and thanking Dr. Krohe for his leadership.
Source: Dr. Mark Krohe with permission from Dr. Carl Buoy
Dr. Michael Todd has implemented quantitative train of four monitoring at multiple academic institutions. His key takeaway:
…most crucial, is that persistent effort is required on the part of departmental leadership (and senior staff). Simply providing equipment, sending out a few messages, and expecting change to occur are unlikely to succeed [5].
Adopting the ASA guidelines will require patience, access to technology, education, internal advocates, and committed leadership. Following the four pillars of implementation, your institution can be victorious and set the standard for others to follow.
Blink Device Company is committed to providing excellent education, hands-on product training, and ongoing support. Our deep clinical understanding and implementation expertise enable us to collaborate with you every step of the way. We offer customized educational programs for partners of all sizes - from small community hospitals to academic institutions and large multi-hospital networks.
Let's work together and make a difference in patient safety! Contact us today.
- Thomas Fuchs-Buder, Edoardo De Robertis, Stephan R. Thilen, Michael W. Champeau; Joint Letter to the Editor from the American Society of Anesthesiologists and the European Society of Anaesthesiology and Intensive Care on Management of Neuromuscular Blockade. Anesthesiology2023; 139:366–367 doi: https://doi.org/10.1097/ALN.0000000000004630
- Fuchs-Buder T, Romero CS, Lewald H, Lamperti M, Afshari A, Hristovska A-M, Schmartz D, Hinkelbein J, Longrois D, Popp M, de Boer HD, Sorbello M, Jankovic R, Kranke P: Peri-operative Management of Neuromuscular Blockade: A Guideline From the European Society of Anaesthesiology and Intensive Care. Eur J Anaesthesiol 2023; 140:82–94
- Edwards LM, Ly NK, Shinefeld J, Morewood GH. (2021), Universal Quantitative Neuromuscular Blockade Monitoring at an Academic Medical Center—A Multimodal Analysis of the Potential Impact on Clinical Outcomes and Total Cost of Care. Perioperative Care and Operating Room Management, Volume 24,100184, ISSN 2405-6030, https://doi.org/10.1016/j.pcorm.2021.100184.
- Santapuram, P., Coker Fowler, L., Garvey, K. V., McEvoy, M. D., Robertson, A., Dunworth, B., McCarthy, K., Freundlich, R., Allen, B. F. S., & Kertai, M. D. (2023). Improving Compliance With Institutional Performance on Train of Four Monitoring. The journal of education in perioperative medicine: JEPM, 25(1), E698. https://doi.org/10.46374/volxxv_issue1_kertai
- Todd, M. M., Hindman, B. J., & King, B. J. (2014). The Implementation of Quantitative Electromyographic Neuromuscular Monitoring in an Academic Anesthesia Department. Anesthesia and Analgesia, 119(2), 323–331. https://doi.org/10.1213/ANE.0000000000000261
- Naguib M, Brull SJ, Hunter JM, Kopman AF, Fülesdi B, Johnson KB, Arkes HR. Anesthesiologists' Overconfidence in Their Perceived Knowledge of Neuromuscular Monitoring and Its Relevance to All Aspects of Medical Practice: An International Survey. Anesth Analg. 2019 Jun;128(6):1118-1126. doi: 10.1213/ANE.0000000000003714. PMID: 31094776.
Implementation
With you every step of the way
Our sole focus is advancing the quality and use of quantitative neuromuscular monitors. To enable the success of our hospital partners, we've developed an implementation pathway and multi-part training that we will tailor to your institution’s goals and needs.
Submit a request to start your customized plan and your regional representative will be in touch shortly. Contact us today!