How to Monitor Succinylcholine-Induced Neuromuscular Blockade

While succinylcholine is generally used for intubation due to its rapid onset and ultrashort duration of action, it can also be administered as an infusion for continuous neuromuscular blockade.
Succinylcholine Infusion for Continuous Relaxation
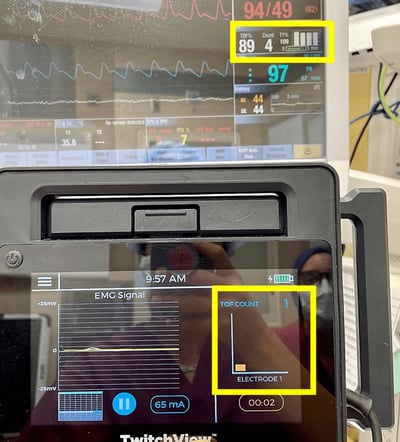
The following case write-up details a succinylcholine drip to maintain relaxation during a bronchial stent removal in a 30-year-old male with chronic respiratory disease. TwitchView, an EMG-based quantitative neuromuscular monitor, guided depolarizing blockade maintenance and extubation. After propofol induction, a baseline measurement was taken on the TwitchView. A 1.0 mg/kg intubation dose of succinylcholine was administered, resulting in a decrease and complete disappearance of all four twitches. In patients with normal plasma cholinesterase levels, succinylcholine-induced block lasts 6 to 13 minutes [1]. Per the ASA guidelines, TwitchView was switched to the single twitch monitoring mode to assess recovery.
The only way to effectively monitor both normal and abnormal succinylcholine-induced neuromuscular blockade is by measuring a single twitch baseline height and using the percentage of that single twitch to gauge return of strength [2].
What is Single Twitch Monitoring?
The single twitch stimulation pattern applies supramaximal stimuli at frequencies ranging from 0.1 Hz (one stimulus every 10 seconds) to 1.0 Hz (one stimulus per second) [1, 3]. Patient responses are compared to the pre-paralytic baseline and expressed as a percentage—for example, a response of one-tenth of the baseline equals T = 10% T1. The TwitchView repeat interval was set to 10 seconds. Once the patient recovered from the intubation dose (T=100%), the anesthesiologist began a 0.1 mg/kg/min succinylcholine infusion, adjusted to maintain T = 20% T1 for optimal surgical condsssions (see Figure 1). After 51 minutes, the case concluded, and the drip was stopped. Patient recovery, indicated by an increasing T value, occurred within four minutes (see Figure 2).


Figures 1 & 2
Images of TwitchView Single Twitch monitoring mode displaying control (bright blue) vs real-time (orange) single twitch responses. Figure 1 on the left depicts an intraoperative measurement of T=20% and Figure 2 on the right depicts patient recovery, T=96%.
Source: author
Large boluses or infusions of succinylcholine can lead to tachyphylaxis and phase II block in individuals with normal plasma cholinesterase activity [1, 3, 4]. Ramsey et al. observed significant interpatient variability in the onset of phase II block during succinylcholine infusions, with the earliest onset occurring after a 2.3 mg/kg dose, while one patient did not develop phase II block until 17.9 mg/kg was given.
What is Phase II Block?
Conventional literature describes depolarizing-induced neuromuscular blockade in two phases. Phase I involves the simultaneous reduction and disappearance of all four twitches at onset and recovery without fade, while Phase II shows fade after tetanic or train of four stimulation and post-tetanic potentiation [1, 2, 3]. However, studies have challenged these definitions, showing fade at both onset and recovery after a single succinylcholine dose [5]. Regardless of how the block is characterized, ensuring adequate recovery before extubation is essential. To confirm the absence of clinically significant fade, the TwitchView monitor was switched from single twitch to train of four mode. A TOFR of 92% indicated minimal fade and adequate recovery (TOFR ≥ 90%) for extubation.

Figure 3: Image of TwitchView train of four monitoring mode displaying patient recovery, TOFR=92%.
Source: author
In a study to determine the prevalence of “phase II” block, defined as a TOFR < 50%, Chen et al. found 33% (5 out of 15 patients) experienced the phenomenon after a similar succinylcholine infusion rate, case length, and anesthetic technique [6]. Inhalation agents like isoflurane can potentiate depolarizing block due to increased muscle blood flow [8, 9]. While "phase II" reversal with an anticholinesterase inhibitor is documented [4, 8, 9], modern practitioners advise caution due to the risk of prolonging the block if succinylcholine remains and the unpredictable response in patients with abnormal pseudocholinesterase activity [1].
How Common is Pseudocholinesterase Deficiency?
Pseudocholinesterase (butyrylcholinesterase) deficiency is an inherited or acquired condition marked by reduced production of the pseudocholinesterase enzyme in the liver. Patients with this deficiency metabolize succinylcholine and mivacurium poorly, leading to prolonged muscle paralysis after standard doses and an increased risk of awareness. The inherited form has two variants: heterozygous, affecting 1 in 500 individuals, and homozygous, affecting 1 in 3,200. Acquired deficiency can arise from conditions like malnutrition, liver disease, cardiac disease, renal disease, cancer, extensive burns, serious infections, pregnancy, or from certain drugs, including steroids, that reduce enzyme production. Clinical manifestations vary widely, with some patients recovering in minutes and others taking several hours. In 1978, Orpollo measured serum cholinesterase levels in 2,215 surgical patients, finding that 5.35% had abnormally low levels [10]. Pseudocholinesterase deficiency may be underappreciated, as it is significantly more common than malignant hypothermia.
Monitor the Effects of Depolarizing Neuromuscular Blocking Agents
Neuromuscular monitors, like TwitchView should be used to confirm patient recovery from succinylcholine before administering non-depolarizing drugs to rule out the presence of a pseudocholinesterase deficiency and to confirm recovery before extubation [1]. If an undiagnosed deficiency occurs, the ASA guidelines recommend quantitative monitoring to guide extubation timing [2]. Using neuromuscular monitoring in patients suspected of having a pseudocholinesterase deficiency is linked to fewer respiratory complications and reduced incidence of awareness [11].
- Naguib, M., Brull, S.J. and Johnson, K.B. (2017), Conceptual and technical insights into the basis of neuromuscular monitoring. Anaesthesia, 72: 16-37.
- Stephan R. Thilen, Wade A. Weigel, Michael M. Todd, Richard P. Dutton, Cynthia A. Lien, Stuart A. Grant, Joseph W. Szokol, Lars I. Eriksson, Myron Yaster, Mark D. Grant, Madhulika Agarkar, Anne M. Marbella, Jaime F. Blanck, Karen B. Domino; 2023 American Society of Anesthesiologists Practice Guidelines for Monitoring and Antagonism of Neuromuscular Blockade: A Report by the American Society of Anesthesiologists Task Force on Neuromuscular Blockade. Anesthesiology 2023; 138:13–41.
- Viby-Mogensen J. (2001). Neuromuscular monitoring. Current opinion in anaesthesiology, 14(6), 655–659.
- Ramsey, Frederic M. MD*; Lebowitz, Philip W. MD*; J, John Savarese, MD†; Ali, Hassan H. MD‡. Clinical Characteristics of Long-Term Succinylcholine Neuromuscular Blockade during Balanced Anesthesia. Anesthesia & Analgesia 59(2):p 110-116, February 1980.
- Naguib, Mohamed MB, BCh, MSc, FFARCSI, MD*; Lien, Cynthia A. MD†; Aker, John CRNA, MS*; Eliazo, Rudolfo BA†. Posttetanic Potentiation and Fade in the Response to Tetanic and Train-of-Four Stimulation During Succinylcholine-Induced Block. Anesthesia & Analgesia 98(6):p 1686-1691, June 2004.
- Chen YA, Fan SZ, Lee PC, Shi JJ, Tsai YC, Chang CL, Liu CC. Continuous succinylcholine infusion and phase II block in short surgical procedures. Ma Zui Xue Za Zhi. 1993 Dec;31(4):253-6. PMID: 8302152.
- Trujillo R, West WP. Pseudocholinesterase Deficiency. [Updated 2023 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan
- Donati F, Bevan DR. Long-term succinylcholine infusion during isoflurane anesthesia. Anesthesiology. 1983 Jan;58(1):6-10.
- Ronald D. Miller, Walter L. Way, William M. Dolan, Wendell C. Stevens, Edmond I. Eger; Comparative Neuromuscular Effects of Pancuronium, Gallamine, and Succinylcholine during Forane and Halothane Anesthesia in Man. Anesthesiology 1971; 35:509–514
- Anthony T. Oropollo; Abnormal Pseudocholinesterase Levels in a Surgical Population. Anesthesiology 1978; 48:284–285
- Andersson ML, Møller AM, Wildgaard K. Butyrylcholinesterase deficiency and its clinical importance in anaesthesia: a systematic review. Anaesthesia. 2019 Apr;74(4):518-528. doi: 10.1111/anae.14545. Epub 2019 Jan