How to Use Post-Tetanic Count (PTC) to Manage Neuromuscular Blockade

What is PTC?
PTC (post-tetanic count) is a neuromuscular monitoring mode that allows the anesthesia care team to assess deep neuromuscular blockade when the TOF Count is 0. PTC monitoring is especially helpful during laparoscopic and robotic-assisted surgeries, where maintenance of deep neuromuscular blockade can be necessary to ensure optimal surgical conditions and patient safety. In the PTC sequence, 50 Hz stimulation is applied for 5 seconds to enhance the neuromuscular junction's response to stimuli. After a three-second pause, single twitches are repeated every second, with the number of responses indicating the PTC (Figure 2). The PTC typically ranges from 0 to 20, with lower numbers indicating deeper blockade [1, 2].
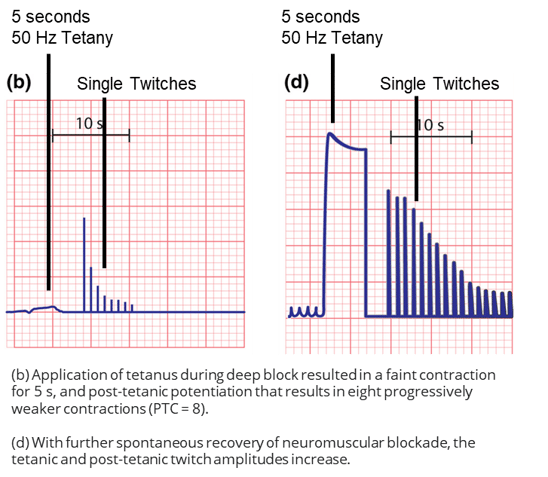 Figure 2: EMG tracing of tetanic stimulation and post-tetanic count during deep neuromuscular blockade (b) and after spontaneous recovery (d) [1].
Figure 2: EMG tracing of tetanic stimulation and post-tetanic count during deep neuromuscular blockade (b) and after spontaneous recovery (d) [1].
Viby-Mogensen et al. developed the post-tetanic sequence after discovering the phenomenon of post-tetanic potentiation, the ability to briefly elicit a response to single-twitch stimuli following high-frequency (tetanic) stimulation. As the patient recovers, the number of responses increases [3]. Typically, a .6mg/kg intubation dose of rocuronium will cause loss of all 4 twitches dropping to PTC, but how long does it take a patient to recover the response to TOF?
Perfusion, potentiating drugs and other factors lead to highly variable patient responses to neuromuscular blocking agents [1]. Debaene determined that the clinical duration of a typical intubation dose of rocuronium (0.6 mg/kg) can range from 15 to 85 minutes [4]. Post-tetanic count offers insights into a patient's rate of spontaneous recovery well before they recover the first TOF twitch allowing anesthesia providers to predict recovery and proactively maintain optimal surgical conditions. In a 2007 BJA article, Dhonneur et al. provide evidence that a PTC measurement of the adductor pollicis is a better early indicator of diaphragmatic recovery than a train-of-four count at corrugator supercilii [5].
Why is PTC Useful?
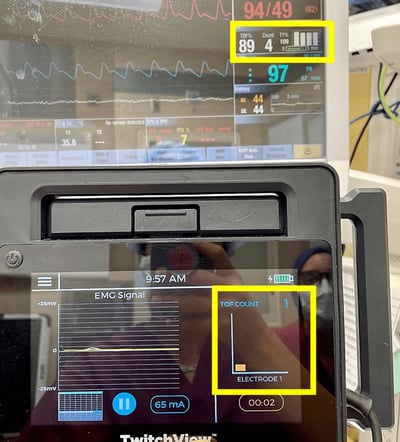
Beyond proactive intervention, PTC can guide anesthesia providers in determining the appropriate clinical intervention. For example, the surgeon indicates that the patient is breathing and requests more rocuronium, will a redose of roc effectively suppress respiration? Some patients retain diaphragmatic function at deep levels of blockade. See Figure 1 for an example of a patient overbreathing the ventilator when they have a PTC of 2. This ability to breathe spontaneously, maintain normal tidal volumes and end-tidal CO2 while deeply relaxed is well documented [6, 7, 8, 9 ].
In the textbook Monitoring in Anesthesia and Perioperative Care, Dr. Aaron Kopman discusses potential clinical response to diaphragmatic recovery.
It is not uncommon to see spontaneous respiration resume at a time when twitch depression at the hand is still quite profound. Thus, the resumption of respiratory effort by itself should not be considered a signal that muscle relaxation is inadequate and that additional blocking agents should be administered. More often than not what the patient is “requesting” is augmented ventilation or supplementary doses of opioid and/or hypnotic. Perhaps all three [9].
Using PTC, you can determine each patient's recovery threshold and set a redosing target. If your patient begins breathing at a PTC 14 or TOFC 1, a proactive redose of neuromuscular blocking agent may be considered. However, if your patient’s recovery threshold resembles the patient in Figure 1, an alternate intervention, as noted by Dr. Kopman may be more effective at suppressing respiration.
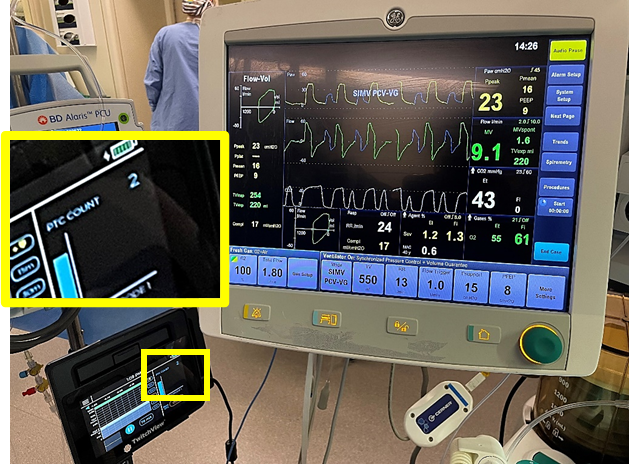 Figure 1: Image showing patient spontaneous breathing, 43 mmHg EtCO2 and 550 ml tidal volume alongside a PTC of 2 on the Twitchview monitor. Source: Author
Figure 1: Image showing patient spontaneous breathing, 43 mmHg EtCO2 and 550 ml tidal volume alongside a PTC of 2 on the Twitchview monitor. Source: Author
TwitchView, an electromyographic neuromuscular monitor, streamlines workflow with AutoPTCTM, an automatic measurement mode based on the patient's real-time level of blockade. When enabled, TwitchView automatically switches between TOF and PTC measurement modes during recovery and after redosing, providing continuous insights into the individual patient.

Figure 3: Auto-PTCTM sequence on the TwitchView Monitor facilitates automatic switching between TOF and PTC monitoring modes. Image source: author
Learn how continuous neuromuscular monitoring can reduce the need for reversal antagonism below.
- Naguib, M., Brull, S.J. and Johnson, K.B. (2017), Conceptual and technical insights into the basis of neuromuscular monitoring. Anaesthesia, 72: 16-37.
- Viby-Mogensen J, Howardy-Hansen P, Chræmmer-Jorgensen B, Ørding H, Engbæk J,
Nielsen A. Posttetanic Count (PTC): a new method of evaluating an intense nondepolarizing
block. Anesthesiology 1981; 55:458-461 - Naguib M, Brull SJ, Kopman AF, et al. Consensus statement on perioperative use of neuromuscular monitoring. Anest Analg. 2018:127(1):71-80.
- Debaene B, Plaud B, Dilly M-P, Donati, F. Residual paralysis in the PACU after a single intubating dose of nondepolarizing muscle relaxant with an intermediate duration of action. Anesthesiology 2003;98:1042-1048.
- Dhonneur G, Kirov K, Motamed C, Amathieu R, Kamoun W, Slavov V, Ndoko SK. Post-tetanic count at adductor pollicis is a better indicator of early diaphragmatic recovery than train-of-four count at corrugator supercilii. Br J Anaesth. 2007 Sep;99(3):376-9. doi: 10.1093/bja/aem124. Epub 2007 Jun 7. PMID: 17561516.
- Fernando PU, Viby-Mogensen J, Bonsu AK, et al. Relationsip between posttetanic count and response to carinal stimulation during vecuronium-induced neuromuscular blockade. Acta Anaesthesiol Scand. 1987;31:593–6.
- Murphy, Glenn S. MD; Szokol, Joseph W. MD. Monitoring Neuromuscular Blockade. International Anesthesiology Clinics 42(2):p 25-40, Spring 2004.
- Donati, F. Residual paralysis: a real problem or did we invent a new disease?. Can J Anesth/J Can Anesth 60, 714–729 (2013).
- Kopman, A. F. (2011). Perioperative Monitoring of Neuromuscular Function. In Monitoring in Anesthesia and Perioperative Care (pp. 261–280). Cambridge University Press.